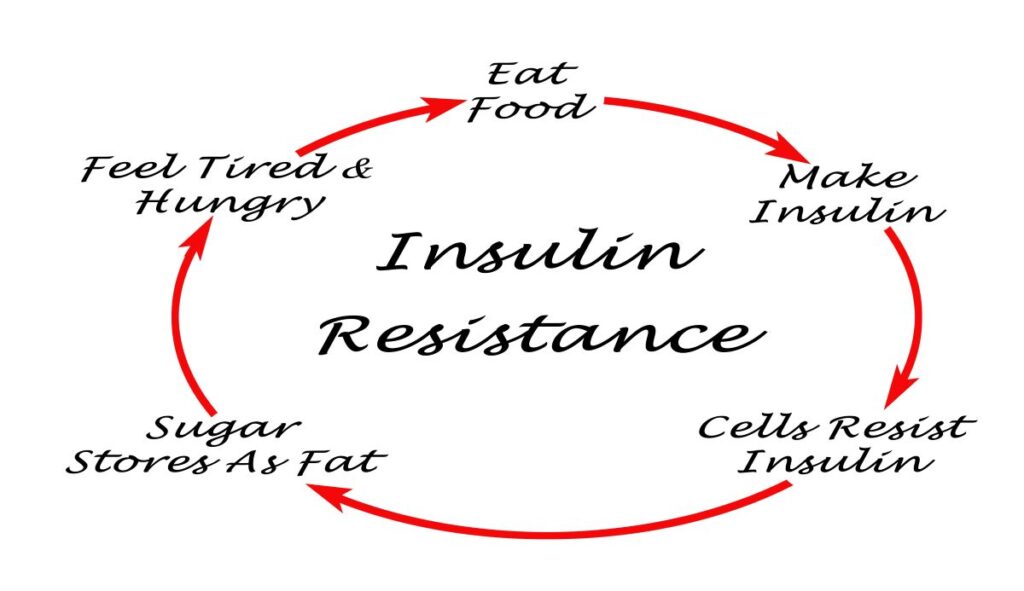
Insulin resistance occurs when your body’s cells become less responsive to insulin, the hormone responsible for moving sugar (glucose) from your bloodstream into your cells for energy. To compensate, your pancreas produces more insulin to keep blood sugar levels stable.
Over time, this overproduction can result in consistently high insulin levels, known as hyperinsulinemia. If left unchecked, this process can progress to prediabetes or type 2 diabetes. Recognizing and addressing insulin resistance early is critical to reduce risk of long-term complications.
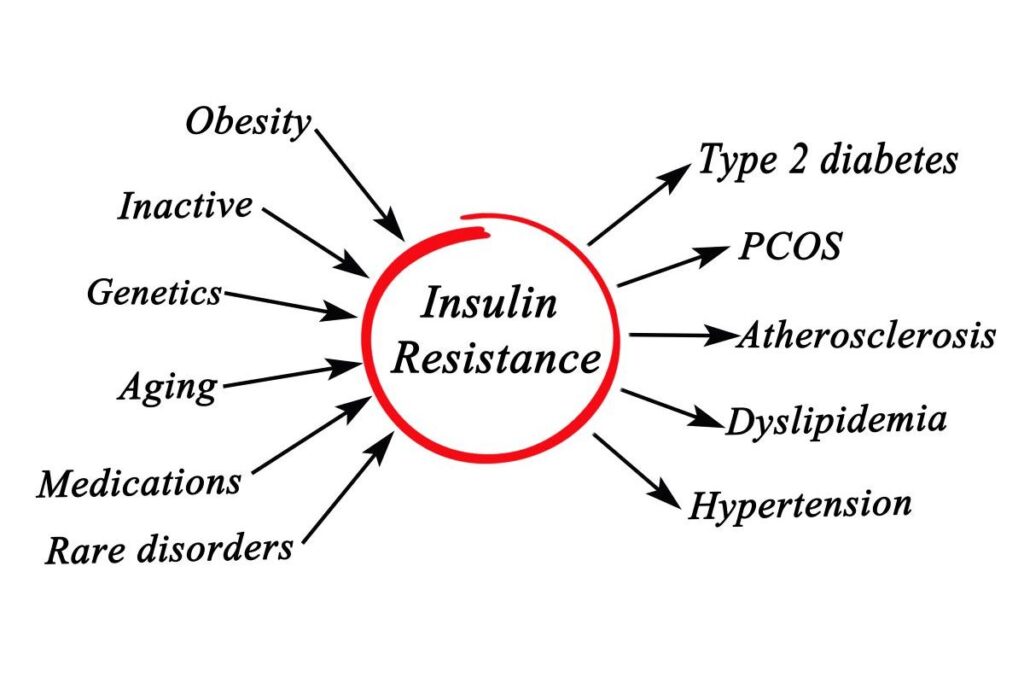
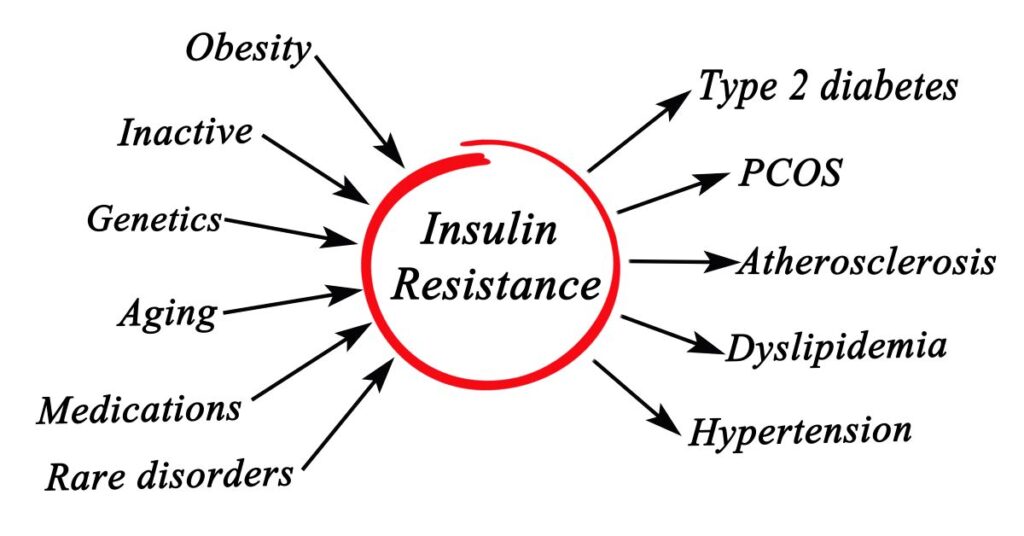
Why Does Insulin Resistance Happen?
Several factors contribute to the development of insulin resistance. These often include:
- Dietary Choices: Consuming large amounts of processed foods and added sugars overwhelms the body with glucose (not to mention inflammation!!), forcing the pancreas to produce more insulin.
- Physical Inactivity: Physical inactivity may reduce the efficiency of muscles in utilizing glucose, potentially affecting insulin function.
- Excess Abdominal Fat: Abdominal fat tissue can release substances that may impact insulin signaling.
- Chronic Stress: Elevated cortisol levels, associated with stress, can affect the body’s glucose processing.
- Other Factors: Age, medications, lipotoxicity and genetics.
These factors often overlap, creating a cycle that can make insulin resistance progressively harder to reverse.
How Insulin Resistance Affects Your Body
Insulin resistance doesn’t just affect blood sugar—it has far-reaching impacts on your overall health. Inefficient glucose utilization by cells may result in elevated blood glucose levels, which can contribute to feelings of fatigue after meals. High insulin levels also promote fat storage, particularly around the abdomen, which is linked to greater health risks. Chronic insulin resistance is associated with low-grade inflammation and may elevate the risk of heart disease, fatty liver disease, and other metabolic disorders.
Recognizing the Early Signs
Insulin resistance often develops without obvious symptoms, but there are subtle indicators to watch for:
- Darkened Skin Patches: Acanthosis nigricans, dark, velvety patches of skin around the neck or armpits, is a common marker.
- Persistent Fatigue: Experiencing fatigue after meals could suggest that cells are not utilizing glucose efficiently.
- Cravings: Intense hunger for sugary or carb-heavy foods can signal imbalances in how your body processes glucose.
In the book Why We Get Sick, a straightforward questionnaire is provided to help assess your risk for insulin resistance. The questions include:
- Do you have more fat around your belly than you’d like?
- Do you have high blood pressure?
- Do you have a family history of heart disease?
- Do you have high levels of blood triglycerides?
- Do you retain water easily?
- Do you have patches of darker-colored skin or little bumps of skin (aka “skin tags”) at your neck, armpits or other areas?
- Do you have a family member with insulin resistance or type 2 diabetes?
- Do you have PCOS or erectile dysfunction?
According to the book, answering “yes” to one question suggests you likely have insulin resistance. If you answered “yes” to two or more, the likelihood is even greater.
How to Address Insulin Resistance
The good news is that insulin resistance can often be improved with targeted lifestyle changes:
- Focus on Whole Foods: Choose vegetables, healthy fats, and proteins while avoiding sugary and processed foods.
- Get Active: Engage in regular physical activity, such as walking, 20 minute at-home workout, or strength training, to help muscles use glucose more effectively.
- Manage Stress: Techniques like yoga, meditation, or deep breathing can reduce cortisol levels and improve insulin sensitivity.
- Prioritize Sleep: Aim for seven to nine hours of quality sleep each night to give your body time to regulate hormones.
These small but impactful changes can make a significant difference over time.
Why Understanding Insulin Resistance Matters
Insulin resistance is often the first warning sign of more serious conditions like type 2 diabetes and cardiovascular disease. Addressing it early can prevent these complications and improve overall health.
By understanding its causes and effects, you can take actionable steps to support your body’s ability to regulate blood sugar effectively. Prevention starts with awareness, and every step you take can contribute to better long-term health.
Disclaimer:
These statements have not been evaluated by the Food and Drug Administration. The content of this article, provided by Addressing Diabetes, is for informational purposes only and does not constitute medical advice. It is not a substitute for professional advice, diagnosis, or treatment. Always consult a qualified healthcare provider with questions about medical conditions, dietary changes, or lifestyle modifications.
The information provided is intended for a general audience and may not apply to individual circumstances. Do not delay or disregard medical advice based on the content of this website. Addressing Diabetes (Holistic Fit LLC) assumes no responsibility for errors, omissions, or outcomes resulting from the use of this information. This content is provided “as is” without guarantees of completeness, accuracy, or timeliness.
The author is not a licensed medical professional. References to specific products, research, or external websites are for informational purposes only and do not constitute endorsements or recommendations. Individual results may vary. Readers are encouraged to consult updated sources and verify information as scientific knowledge evolves.
References:
https://pmc.ncbi.nlm.nih.gov/articles/PMC8831809
https://pmc.ncbi.nlm.nih.gov/articles/PMC9505491
https://pubmed.ncbi.nlm.nih.gov/33775061
https://medicine.yale.edu/news-article/how-to-reverse-insulin-resistance
https://www.ncbi.nlm.nih.gov/books/NBK507839
Bikman, B. (2020). Why we get sick: The hidden epidemic at the root of most chronic disease—and how to fight it. Dallas: BenBella Books, Inc.